Noticing blood in stools can be a frightening experience. It’s one of those symptoms that immediately raises concern, often leading people to think about colon cancer. While this association isn’t entirely wrong—since blood in stools can be a sign of colon cancer—it’s important to understand that not all cases point to a life-threatening diagnosis. There are many possible causes, ranging from minor to serious, and understanding the context is key to knowing when to seek medical help.
What Does Blood in Stools Indicate?
Rectal bleeding can present itself in various ways, depending on where the bleeding originates within the digestive tract. If the blood is bright red and appears on the toilet paper or surface of the stool, it usually indicates bleeding from the lower rectum or anus. This is often caused by conditions such as hemorrhoids or anal fissures.
On the other hand, if the stool appears dark or tarry, it may suggest bleeding from the upper gastrointestinal tract, including the stomach or small intestine. Sometimes, the bleeding is so small it’s not visible to the naked eye and can only be detected through specialized tests such as a fecal occult blood test (FOBT). Whether visible or hidden, blood in the bowel should always be evaluated, especially if it persists.
Common Non-Cancerous Causes
There are several benign or non-cancerous reasons for blood in stools. Hemorrhoids, which are swollen veins in the rectum or anus, are one of the most common causes. They can rupture and bleed, especially after straining during bowel movements. Anal fissures—small tears in the skin of the anus—can also cause bright red bleeding, often accompanied by pain during defecation.
Other possible causes include diverticulosis, where small pouches in the colon wall become inflamed or infected; inflammatory bowel diseases such as Crohn’s disease and ulcerative colitis; and gastrointestinal infections that cause inflammation and bleeding. These conditions may be uncomfortable or even painful but are generally not life-threatening if treated early.
Colon Cancer: A Serious Possibility
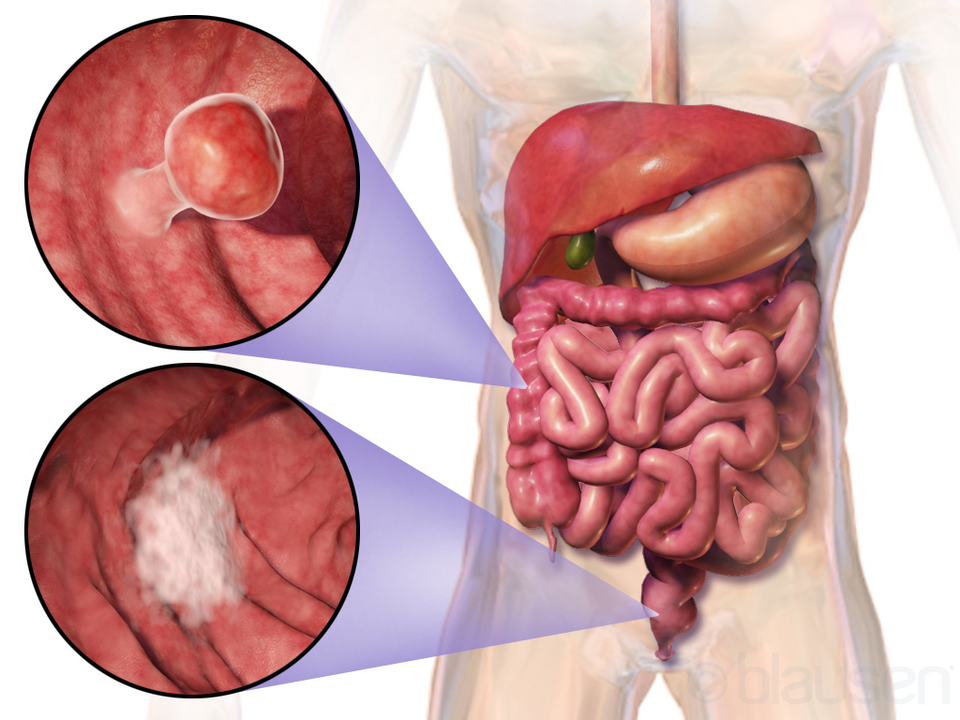
While many cases of blood in stools are not cancer, the possibility cannot be overlooked. Colon cancer remains one of the leading causes of cancer-related deaths worldwide. It usually develops slowly over time, often starting from benign polyps that may eventually become cancerous. These polyps can bleed occasionally, making rectal bleeding one of the earliest warning signs of colon cancer.
However, colon cancer often presents with a combination of symptoms, not just blood in stools. Other warning signs include a persistent change in bowel habits (such as chronic constipation or diarrhea), abdominal discomfort or bloating, unexplained weight loss, fatigue, and the feeling that your bowel doesn’t empty completely. When any of these occur together, they warrant prompt medical attention.
When Should You See a Doctor?
If you notice blood in stools more than once or experience ongoing gastrointestinal discomfort, it’s time to see a healthcare professional. Even if the bleeding seems minor, you should not ignore it, especially if it recurs or is accompanied by other symptoms like abdominal pain, fatigue, or changes in stool consistency.
Doctors may begin with a physical exam and review of your symptoms. You might undergo a stool test to detect hidden blood or signs of infection. In many cases, a colonoscopy is the most definitive way to identify the cause of bleeding. It allows direct visualization of the colon and the opportunity to remove polyps or take biopsies if needed.
Preventive Measures and Lifestyle Factors
Fortunately, there are steps you can take to lower your risk of gastrointestinal problems, including colon cancer. A diet rich in fiber—fruits, vegetables, legumes, and whole grains—helps keep your digestive system healthy. Reducing your intake of processed and red meats, avoiding smoking, and limiting alcohol consumption also reduce your risk. Regular physical activity supports overall health and may lower the risk of bowel cancer.
It’s also helpful to maintain regular bowel habits. Straining during bowel movements increases the likelihood of developing hemorrhoids and anal fissures. Drinking plenty of water and staying physically active can promote softer stools and easier digestion.
Conclusion
In summary, while blood in stools can be a symptom of colon cancer, it is not always the case. Many other medical conditions—some mild and others more serious—can cause rectal bleeding. What’s crucial is not to ignore this symptom or make assumptions. A timely consultation with a healthcare provider and appropriate testing are essential to identify the root cause and ensure appropriate treatment.
Whether the cause is minor or serious, early evaluation and regular screening are your best defenses. If you’ve seen blood in your stool or are overdue for a screening, now is the time to take action. Prioritizing your digestive health could make all the difference.







